BABESIA
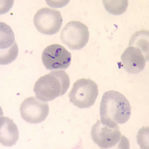
Babesia is a red blood cell parasite that belongs to the Apicomplexa phylum, a group of parasitic organisms which also includes other piroplasms such as Theileria and the Plasmodium species that are the causative organisms underlying malaria. Infection from the Babesia parasite is known as Babesiosis, a malarial-like disease (2). Babesia is one of the most common animal parasites in the world (3), with over 100 species identified to date. Each species is broadly classified by numerous factors, including organism size and reservoir host, though the natural host is not always able to be identified (2).
A number of Babesia species have been found to be pathogenic to humans, with both the small and large Babesia parasites being able to cause illness in humans. The large Babesia species include bovine parasites B. divergens, B. bovis, B. bigemina, deer parasite B. venatorum and canine parasite B.canis. The smaller Babesia species include the rodent parasite B. microti, and B duncani (previously known as WA1). Although B. duncani has been found in the blood of sick humans, no natural reservoir host or tick vector has been identified for this species as yet. Of these Babesia species, the four main ones that have been identified as underlying human Babesiosis are, B. microti, B. duncani, B. divergens and B. venatorum, with B. bigemina, B.bovis and B. canis, also being implicated in a number of cases of human infection (3-8).
B. bovis and B. bigemina are believed to have been introduced into Australia around 1872, the same time as the cattle tick (9, 10), with over 80% of tick fever outbreaks in Australia due to B. bovis (11). The first known case of human Babesia in Australia came to light as the result of a Babesia microti infection and subsequent death of a 56yo NSW male in April 2011 (12, 13). Babesia microti is not endemic to Australia; rather it is an American species of Babesia. Research on how these protozoa came to be in the Australian environment, and how someone contracted it, and subsequently died, still does not appear to have garnered research or public education with regards to Babesia in Australia.
It should also be noted that a Babesia infection can be passed from mother to foetus (14-17). Babesia protozoa are also able survive in stored blood and be passed on through blood transfusions (17-19).
A number of Babesia species have been found to be pathogenic to humans, with both the small and large Babesia parasites being able to cause illness in humans. The large Babesia species include bovine parasites B. divergens, B. bovis, B. bigemina, deer parasite B. venatorum and canine parasite B.canis. The smaller Babesia species include the rodent parasite B. microti, and B duncani (previously known as WA1). Although B. duncani has been found in the blood of sick humans, no natural reservoir host or tick vector has been identified for this species as yet. Of these Babesia species, the four main ones that have been identified as underlying human Babesiosis are, B. microti, B. duncani, B. divergens and B. venatorum, with B. bigemina, B.bovis and B. canis, also being implicated in a number of cases of human infection (3-8).
B. bovis and B. bigemina are believed to have been introduced into Australia around 1872, the same time as the cattle tick (9, 10), with over 80% of tick fever outbreaks in Australia due to B. bovis (11). The first known case of human Babesia in Australia came to light as the result of a Babesia microti infection and subsequent death of a 56yo NSW male in April 2011 (12, 13). Babesia microti is not endemic to Australia; rather it is an American species of Babesia. Research on how these protozoa came to be in the Australian environment, and how someone contracted it, and subsequently died, still does not appear to have garnered research or public education with regards to Babesia in Australia.
It should also be noted that a Babesia infection can be passed from mother to foetus (14-17). Babesia protozoa are also able survive in stored blood and be passed on through blood transfusions (17-19).
For information on Symptoms of Babesiosis see:
What is Lyme: Babesia Symptoms
Babesia Microti Transcript by Jessica and Jennifer
What is Lyme: Babesia Symptoms
Babesia Microti Transcript by Jessica and Jennifer
References: CO-INFECTIONS: Babesia
Please note: Any information with regards to Lyme disease that is freely available at numerous locations on the internet has not been referenced. For specific facts/arguments, see the reference list.
NB: Reference section is separated into segments for ease of updating information
NB: Reference section is separated into segments for ease of updating information
Reference 1 can be seen / is relevant to the Role of Mammals as Vector and Reservoir Hosts in Borrelia (Lyme) section when discussing the multiple pathogens carried by H. longicornis ticks
(1) Thompson C, Spielman A, Krause PJ (2001) Coinfecting deer-associated zoonoses: Lyme disease, babesiosis, and ehrlichiosis. Clin Infect Dis. 2001 Sep 1;33(5):676-85. Epub 2001 Aug 6. http://www.ncbi.nlm.nih.gov/pubmed/11486290
Babesia
(2) Yabsley MJ and Shock BC (2012) Natural history of Zoonotic Babesia: Role of wildlife reservoirs. Int J Parasitol Parasites Wildl. Nov 22;2:18-31 http://www.ncbi.nlm.nih.gov/pubmed/24533312
(3) Homer MJ, Aguilar-Delfin I, Telford SR 3rd, Krause PJ, Persing DH (2000) Babesiosis. Clin Microbiol Rev. Jul;13(3):451-69. http://www.ncbi.nlm.nih.gov/pubmed/10885987
(4) Bovine Babesiosis. Centre for Food Security and Public Health 2008. http://www.cfsph.iastate.edu/Factsheets/pdfs/bovine_babesiosis.pdf
(5) Infection With Various Protozoa: Babesia. Distance Learning Lecture Notes.
http://www.itg.be/itg/distancelearning/lecturenotesvandenendene/08_Various_protozoap13.htm
(6) Hunfeld KP, Hildebrandt A and Gray JS (2008) Babesiosis: Recent insights into an ancient disease. Int J Parasitol; 38: 1219–1237. http://www.nslc.wustl.edu/courses/Bio348/thach/2011/Babesiosis%20review.pdf
(7) Human Babesiosis. Abelardo C. Moncayo, Ph.D. 2010 Director, Vector-Borne Diseases, Tennessee Department of Health. http://www.ncagr.gov/oep/oneMedicine/noms/2010/Moncayo_Abelardo_Human_Babesiosis.pdf
(8) Uilenberg G (2006) Babesia – a historical overview. Vet Parasitol; 138(1-2):3-10. Epub 2006 Feb 28
http://www.ncbi.nlm.nih.gov/pubmed/16513280
(9) Angus BM (1996) The history of the cattle tick Boophilus microplus in Australia and achievements in its control. Int J Parasitol: 26(12):1341-1355. http://www.ncbi.nlm.nih.gov/pubmed/9024884
(10) Bock RE, de Vos AJ and Molloy JB. Tick-borne diseases of Cattle. Australian and New Zealand Standard Diagnostic Procedures March 2006
Original article accessed no longer available: Ie: [http://www.scahls.org.au/__data/assets/pdf_file/0008/1280852/tick_borne_diseases.pdf]
See instead: http://www.agriculture.gov.au/SiteCollectionDocuments/animal/ahl/ANZSDP-Tick_borne_diseases.pdf
(11) NSW Department of Primary Industries. Tick Fever: ISSN 1832-6668
http://www.dpi.nsw.gov.au/__data/assets/pdf_file/0005/58289/Tick_fever_-_Primefact_80-final.pdf
(12) Senanayake SN, Paparini A, Latimer M, Andriolo K, Dasilva AJ, Wilson H, Xayavong MV, Collignon PJ, Jeans P and Irwin PJ (2012). First report of human babesiosis in Australia. Med J Aust 196(5):350-352. http://www.ncbi.nlm.nih.gov/pubmed/22432676
https://www.mja.com.au/journal/2012/196/5/first-report-human-babesiosis-australia
(13) First case of babesiosis in Australia baffles scientists. May 2012. Science Network Western Australia: Accessed August 2012. http://www.sciencewa.net.au/topics/health-a-medicine/item/1451-first-case-of-babesiosis-in-australia-baffles-scientists
(14) Esernio-Jenssen D, Scimeca PG, Benach JL, Tenenbaum MJ (1987) Transplacental/perinatal babesiosis. J Pediatr 110(4):570-2 http://www.ncbi.nlm.nih.gov/pubmed/3559805?dopt=Abstract
(15) Feder, HM (2003) Babesiosis in Pregnancy. N Engl J Med ; 349:195-196
http://www.nejm.org/doi/full/10.1056/NEJM200307103490221
(16) Sethi S, Alcid D, Kesarwala H, Tolan RW Jr (2009) Probable Congenital Babesiosis in Infant, New Jersey, USA. Emerg Infect Dis; 15(5): 788–791 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687033/
(17) Joseph JT, Purtill K, Wong SJ, Munoz J, Teal A, Madison-Antenucci S, Horowitz HW, Aguero-Rosenfeld ME, Moore JM, Abramowsky C, Wormser GP (2012) Vertical transmission of Babesia microti, United States. Emerg Infect Dis Aug;18(8):1318-21. http://www.ncbi.nlm.nih.gov/pubmed/22840424
(18) Ngo V and Civen R (2009) Babesiosis Acquired through Blood Transfusion, California, USA. Emerg Infect Dis ; 15(5): 785–787. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687036/
(19) CDC: Babesia in the Blood Supply: Tickborne Parasite Transmitted via Transfusion. Accessed August 2012: http://www.cdc.gov/parasites/features/babesia_article_9-5-11.html
(1) Thompson C, Spielman A, Krause PJ (2001) Coinfecting deer-associated zoonoses: Lyme disease, babesiosis, and ehrlichiosis. Clin Infect Dis. 2001 Sep 1;33(5):676-85. Epub 2001 Aug 6. http://www.ncbi.nlm.nih.gov/pubmed/11486290
Babesia
(2) Yabsley MJ and Shock BC (2012) Natural history of Zoonotic Babesia: Role of wildlife reservoirs. Int J Parasitol Parasites Wildl. Nov 22;2:18-31 http://www.ncbi.nlm.nih.gov/pubmed/24533312
(3) Homer MJ, Aguilar-Delfin I, Telford SR 3rd, Krause PJ, Persing DH (2000) Babesiosis. Clin Microbiol Rev. Jul;13(3):451-69. http://www.ncbi.nlm.nih.gov/pubmed/10885987
(4) Bovine Babesiosis. Centre for Food Security and Public Health 2008. http://www.cfsph.iastate.edu/Factsheets/pdfs/bovine_babesiosis.pdf
(5) Infection With Various Protozoa: Babesia. Distance Learning Lecture Notes.
http://www.itg.be/itg/distancelearning/lecturenotesvandenendene/08_Various_protozoap13.htm
(6) Hunfeld KP, Hildebrandt A and Gray JS (2008) Babesiosis: Recent insights into an ancient disease. Int J Parasitol; 38: 1219–1237. http://www.nslc.wustl.edu/courses/Bio348/thach/2011/Babesiosis%20review.pdf
(7) Human Babesiosis. Abelardo C. Moncayo, Ph.D. 2010 Director, Vector-Borne Diseases, Tennessee Department of Health. http://www.ncagr.gov/oep/oneMedicine/noms/2010/Moncayo_Abelardo_Human_Babesiosis.pdf
(8) Uilenberg G (2006) Babesia – a historical overview. Vet Parasitol; 138(1-2):3-10. Epub 2006 Feb 28
http://www.ncbi.nlm.nih.gov/pubmed/16513280
(9) Angus BM (1996) The history of the cattle tick Boophilus microplus in Australia and achievements in its control. Int J Parasitol: 26(12):1341-1355. http://www.ncbi.nlm.nih.gov/pubmed/9024884
(10) Bock RE, de Vos AJ and Molloy JB. Tick-borne diseases of Cattle. Australian and New Zealand Standard Diagnostic Procedures March 2006
Original article accessed no longer available: Ie: [http://www.scahls.org.au/__data/assets/pdf_file/0008/1280852/tick_borne_diseases.pdf]
See instead: http://www.agriculture.gov.au/SiteCollectionDocuments/animal/ahl/ANZSDP-Tick_borne_diseases.pdf
(11) NSW Department of Primary Industries. Tick Fever: ISSN 1832-6668
http://www.dpi.nsw.gov.au/__data/assets/pdf_file/0005/58289/Tick_fever_-_Primefact_80-final.pdf
(12) Senanayake SN, Paparini A, Latimer M, Andriolo K, Dasilva AJ, Wilson H, Xayavong MV, Collignon PJ, Jeans P and Irwin PJ (2012). First report of human babesiosis in Australia. Med J Aust 196(5):350-352. http://www.ncbi.nlm.nih.gov/pubmed/22432676
https://www.mja.com.au/journal/2012/196/5/first-report-human-babesiosis-australia
(13) First case of babesiosis in Australia baffles scientists. May 2012. Science Network Western Australia: Accessed August 2012. http://www.sciencewa.net.au/topics/health-a-medicine/item/1451-first-case-of-babesiosis-in-australia-baffles-scientists
(14) Esernio-Jenssen D, Scimeca PG, Benach JL, Tenenbaum MJ (1987) Transplacental/perinatal babesiosis. J Pediatr 110(4):570-2 http://www.ncbi.nlm.nih.gov/pubmed/3559805?dopt=Abstract
(15) Feder, HM (2003) Babesiosis in Pregnancy. N Engl J Med ; 349:195-196
http://www.nejm.org/doi/full/10.1056/NEJM200307103490221
(16) Sethi S, Alcid D, Kesarwala H, Tolan RW Jr (2009) Probable Congenital Babesiosis in Infant, New Jersey, USA. Emerg Infect Dis; 15(5): 788–791 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687033/
(17) Joseph JT, Purtill K, Wong SJ, Munoz J, Teal A, Madison-Antenucci S, Horowitz HW, Aguero-Rosenfeld ME, Moore JM, Abramowsky C, Wormser GP (2012) Vertical transmission of Babesia microti, United States. Emerg Infect Dis Aug;18(8):1318-21. http://www.ncbi.nlm.nih.gov/pubmed/22840424
(18) Ngo V and Civen R (2009) Babesiosis Acquired through Blood Transfusion, California, USA. Emerg Infect Dis ; 15(5): 785–787. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687036/
(19) CDC: Babesia in the Blood Supply: Tickborne Parasite Transmitted via Transfusion. Accessed August 2012: http://www.cdc.gov/parasites/features/babesia_article_9-5-11.html